Throat
Doctor, Why Am I Hoarse?
 Insight into causes, prevention, and when to see an ENT
Insight into causes, prevention, and when to see an ENT
What Is It?
Hoarseness is a general term that describes abnormal voice changes. When hoarse, the voice may sound breathy, raspy, strained, or there may be changes in volume (loudness) or pitch (how high or low the voice is). The changes in sound are usually due to disorders related to the vocal cords that are the sound producing parts of the voice box (larynx). While breathing, the vocal cords remain apart. When speaking or singing, they come together, and as air leaves the lungs, they vibrate, producing sound. Swelling or lumps on the vocal cords prevent them from coming together properly and changes the way the cords vibrate, which makes a change in the voice, altering quality, volume, and pitch.
What Are the Causes?
 Acute Laryngitis: There are many causes of hoarseness. Fortunately, most are not serious and tend to go away in a short period of time. The most common cause is acute laryngitis, which usually occurs due to swelling from a common cold, upper respiratory tract viral infection, or irritation caused by excessive voice use such as screaming at a sporting event or rock concert.
Acute Laryngitis: There are many causes of hoarseness. Fortunately, most are not serious and tend to go away in a short period of time. The most common cause is acute laryngitis, which usually occurs due to swelling from a common cold, upper respiratory tract viral infection, or irritation caused by excessive voice use such as screaming at a sporting event or rock concert.
Vocal Nodules: More prolonged hoarseness is usually due to using your voice either too much, too loudly, or improperly over extended periods of time. These habits can lead to vocal nodules (singers’ nodes), which are callous-like growths, or may lead to polyps of the vocal cords (more extensive swelling). Both of these conditions are benign. Vocal nodules are common in children and adults who raise their voice in work or play.
Gastroesophageal Reflux: A common cause of hoarseness is gastro-esophageal reflux, when stomach acid comes up the swallowing tube (esophagus) and irritates the vocal cords. Many patients with reflux-related changes of voice do not have symptoms of heartburn. Usually, the voice is worse in the morning and improves during the day. These people may have a sensation of a lump in their throat, mucus sticking in their throat or an excessive desire to clear their throat.
Smoking: Smoking is another cause of hoarseness. Since smoking is the major cause of throat cancer, if smokers are hoarse, they should see an otolaryngologist.
Other Causes: Many unusual causes for hoarseness include allergies, thyroid problems, neurological disorders, trauma to the voice box, and occasionally, the normal menstrual cycle.
Who Can Treat My Hoarseness?
Hoarseness due to a cold or flu may be evaluated by family physicians, pediatricians, and internists (who have learned how to examine the larynx). When hoarseness lasts longer than two weeks or has no obvious cause it should be evaluated by an otolaryngologist--head and neck surgeon (ear, nose and throat doctor). Problems with the voice are best managed by a team of professionals who know and understand how the voice functions. These professionals are otolaryngologist--head and neck surgeons, speech/language pathologists, and teachers of singing, acting, or public speaking. Voice disorders have many different characteristics that may give professionals a clue to the cause.
How Is Hoarseness Evaluated?
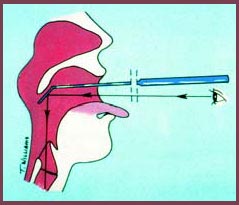
An otolaryngologist will obtain a thorough history of the hoarseness and your general health. Your doctor will usually look at the vocal cords with either a mirror placed in the back of your throat, or a very small, lighted flexible tube (fiberoptic scope) may be passed through your nose in order to view your vocal cords. Videotaping the examination or using stroboscopy (slow motion assessment) may also help with the analysis.
These procedures are not uncomfortable and are well tolerated by most patients. In some cases, special tests (known as acoustic analysis) designed to evaluate the voice, may be recommended. These measure voice irregularities, how the voice sounds, airflow, and other characteristics that are helpful in establishing a diagnosis and guiding treatment
When should I see an otolaryngologist (ENT doctor)?
- Hoarseness lasting longer than two weeks especially if you smoke
- Pain not from a cold or flu
- Coughing up blood
- Difficulty swallowing
- Lump in the neck
- Loss or severe change in voice lasting longer than a few days
How Are Vocal Disorders Treated?
 The treatment of hoarseness depends on the cause. Most hoarseness can be treated by simply resting the voice or modifying how it is used. The otolaryngologist may make some recommendations about voice use behavior, refer the patient to other voice team members, and in some instances recommend surgery if a lesion, such as a polyp, is identified. Avoidance of smoking or exposure to secondhand smoke (passive smoking) is recommended to all patients. Drinking fluids and possibly using medications to thin the mucus are also helpful.
The treatment of hoarseness depends on the cause. Most hoarseness can be treated by simply resting the voice or modifying how it is used. The otolaryngologist may make some recommendations about voice use behavior, refer the patient to other voice team members, and in some instances recommend surgery if a lesion, such as a polyp, is identified. Avoidance of smoking or exposure to secondhand smoke (passive smoking) is recommended to all patients. Drinking fluids and possibly using medications to thin the mucus are also helpful.
Specialists in speech/language pathology (voice therapists) are trained to assist patients in behavior modification that may help eliminate some voice disorders. Patients who have developed bad habits, such as smoking or overuse of their voice by yelling and screaming, benefit most from this conservative approach. The speech/language pathologist may teach patients to alter their method of speech production to improve the sound of the voice and to resolve problems, such as vocal nodules. When a patients' problem is specifically related to singing, a singing teacher may help improve the patients' singing techniques.
What Can I Do to Prevent and Treat Mild Hoarseness?
- • If you smoke, quit.
- Avoid agents that dehydrate the body, such as alcohol and caffeine.
- Avoid secondhand smoke.
- Drink plenty of water.
- Humidify your home.
- Watch your diet–avoid spicy foods.
- Try not to use your voice too long or too loudly.
- Use a microphone if possible in situations where you need to project your voice.
- Seek professional voice training.
- Avoid speaking or singing when your voice is injured or hoarse.
Doctor, I Have Trouble Swallowing
Swallowing Disorders
Difficulty in swallowing (dysphagia) is common among all age groups, especially the elderly. The term dysphagia refers to the feeling of difficulty passing food or liquid from the mouth to the stomach. This may be caused by many factors, most of which are temporary and not threatening. Difficulties in swallowing rarely represent a more serious disease, such as a tumor or a progressive neurological disorder. When the difficulty does not clear up by itself in a short period of time, you should see an otolaryngologist–head and neck surgeon.
How You Swallow
People normally swallow hundreds of times a day to eat solids, drink liquids, and swallow the normal saliva and mucus that the body produces. The process of swallowing has four stages:
- The first is oral preparation, where food or liquid is manipulated and chewed in preparation for swallowing.
- During the oral stage, the tongue propels the food or liquid to the back of the mouth, starting the swallowing response.
- The pharyngeal stage begins as food or liquid is quickly passed through the pharynx, the canal that connects the mouth with the esophagus, into the esophagus or swallowing tube.
- In the final, esophageal stage, the food or liquid passes through the esophagus into the stomach.
Although the first and second stages have some voluntary control, stages three and four occur by themselves, without conscious input.
What Causes Swallowing Disorders?
Any interruption in the swallowing process can cause difficulties. It may be due to simple causes such as poor teeth, ill fitting dentures, or a common cold. One of the most common causes of dysphagia is gastroesophageal reflux. This occurs when stomach acid moves up the esophagus to the pharynx, causing discomfort. Other causes may include: stroke; progressive neurologic disorder; the presence of a tracheostomy tube; a paralyzed or unmoving vocal cord; a tumor in the mouth, throat, or esophagus; or surgery in the head, neck, or esophageal areas.
Symptoms
Symptoms of swallowing disorders may include:
- drooling;
- a feeling that food or liquid is sticking in the throat;
- discomfort in the throat or chest (when gastroesophageal reflux is present);
- a sensation of a foreign body or "lump" in the throat;
- weight loss and inadequate nutrition due to prolonged or more significant problems with swallowing; and
- coughing or choking caused by bits of food, liquid, or saliva not passing easily during swallowing, and being sucked into the lungs.
Who Evaluates and Treats Swallowing Disorders?
When dysphagia is persistent and the cause is not apparent, the otolaryngologist–head and neck surgeon will discuss the history of your problem and examine your mouth and throat. This may be done with the aid of mirrors or a small tube (flexible laryngoscope), which provides vision of the back of the tongue, throat, and larynx (voice box). If necessary, an examination of the esophagus, stomach, and upper small intestine (duodenum) may be carried out by the otolaryngologist or a gastroenterologist. These specialists may recommend X-rays of the swallowing mechanism, called a barium swallow or upper G-I, which is done by a radiologist.
If special problems exist, a speech pathologist may consult with the radiologist regarding a modified barium swallow or videofluroscopy. These help to identify all four stages of the swallowing process. Using different consistencies of food and liquid, and having the patient swallow in various positions, a speech pathologist will test the ability to swallow. An exam by a neurologist may be necessary if the swallowing disorder stems from the nervous system, perhaps due to stroke or other neurologic disorders.
Possible Treatments
Many of these disorders can be treated with medication. Drugs that slow stomach acid production, muscle relaxants, and antacids are a few of the many medicines available. Treatment is tailored to the particular cause of the swallowing disorder.
Gastroesophageal reflux can often be treated by changing eating and living habits, for example:
- eat a bland diet with smaller, more frequent meals;
- eliminate alcohol and caffeine;
- reduce weight and stress;
- avoid food within three hours of bedtime; and
- elevate the head of the bed at night.
If these don't help, antacids between meals and at bedtime may provide relief.
Many swallowing disorders may be helped by direct swallowing therapy. A speech pathologist can provide special exercises for coordinating the swallowing muscles or restimulating the nerves that trigger the swallow reflex. Patients may also be taught simple ways to place food in the mouth or position the body and head to help the swallow occur successfully.
Some patients with swallowing disorders have difficulty feeding themselves. An occupational therapist can aid the patient and family in feeding techniques. These techniques make the patient as independent as possible. A dietician or nutritional expert can determine the amount of food or liquid necessary to sustain an individual and whether supplements are necessary.
Once the cause is determined, swallowing disorders may be treated with:
- medication
- swallowing therapy
- surgery
Surgery is used to treat certain problems. If a narrowing or stricture exists, the area may need to be stretched or dilated. If a muscle is too tight, it may need to be dilated or released surgically. This procedure is called a myotomy and is performed by an otolaryngologist–head and neck surgeon.
Many causes contribute to swallowing disorders. If you have a persistent problem swallowing, see an otolaryngologist–head and neck surgeon.